´
Wolff-Parkinson-WhiteÇóQC[ºp¬«s®¬ÌqóãwK«]¿yÑ»è@ÉÖ·é¢
îàc@MvC§Ô@³ê
hqãÈåwZhqãw¤Z^[Ùí«q¶¤å
A Review of Evaluating and Assessing Aeromedical Fitness of Pilots with Wolff-Parkinson-White Syndrome or Atrioventricular Tachyarrhythmias
Kunio Takada, Shoichi Tachibana
Division of Environmental Medicine, National Defense Medical College Research Institutey
ABSTRACT
@In this review, we defined the mechanisms by which macro-reentry circuits in the atrioventricular region evoke paroxysmal supraventricular tachycardia as gatrioventricular tachyarrhythmias iAVTjh and hemodynamic aberrance, based on AVT as ghemodynamic phenomena iHDPjh.@HDP is an aeromedical concern among pilots who become incapacitated during flight.@The assessment of aeromedical fitness, hereafter referred to as gfitnessh, of the pilot should be performed with caution in order to obtain precise clinical findings.@Herein, we propose methods to evaluate and assess aeromedical fitness of pilots for AVT, based on our review of the literature.
@In cases with a history of HDP, when all of the reentry circuits are presumed as being functional based upon an electrophysiological study iEPSj, in principle the pilot is qualified as exhibiting fitness without restriction, otherwise the pilots are not considered fit.
@In cases with Wolff-Parkinson-White iWPWj syndrome without a history of HDP and EPS, those pilots aged 40 years or more, exhibit fitness restricted to low-G aircraft.@If the pilot is less than 40 years of age, they would have fitness restricted to multicrew operations and low-G aircraft.@To remove the restriction, the following procedures may be performed;1j exhibiting both a QRS≦120 msec and Rosenbaum type B on electrocardiography, which would indicate a fasciculoventricular pathway iFVPj that would not develop to HDP;2j The characteristic waveform is presumed from FVP based on no alteration in the QRS waveform using Holter electrocardiogram or adenosine test;and 3j long anterograde effective refractory period is presumed based on intermittent WPW syndrome or disappearance of the delta wave on exercise testing.@In cases with Lown-Ganong-Levine syndrome, which we defined as sustained PR interval <110 msec despite repeated testing, without a history of HDP and EPS, the pilot would have fitness restricted to multicrew operations and low-G aircraft.@To remove the restriction, the observation of no alteration in the QRS waveform on Holter electrocardiogram or adenosine test, which is presumed as not having any apparent alternative pathway, may be performed.
iReceived:13 July, 2015@Accepted:18 March, 2016j
Key words:Wolff-Parkinson-White syndrome, pre-excitation syndrome, paroxysmal supraventricular tachycardia, aviation medicine, waiver
I.@¾
@㺫ÉdCI»±Ì}NGg[@Éæéì«ãºpiparoxysmal supraventricular tachycardia: PSVTjðN±·¾³ÍCȺÌæ¤ÈñÂÌÇÊɪÞÅ«éB
@@@[ºÔðÔ`±HÍ[ºßðîµÄdCI»±ªùñ·éàÌCÍC»ÌÇÌÂ\«ª éàÌi[ºÌæjB
@A@[àÉÀǵ½dCI»±ðùñ·éàÌiS[jB
@@ ÉY·éàÌÍC[ºßGg[piatrioventricular nodal re-entrant tachycardia:AVNRTjC[ºGg[piatrioventricular re-entrant tachycardia: AVRTjCpermanent form of junctional atrioventricular reciprocating tachycardiaiPJRTjCWolff-Parkinson-WhiteiWPWjÇóQyÑLown-Ganong-LevineiLGLjÇóQÌú»±ÇóQipre-excitation syndrome: PESjª°çêéBȨCPESÍC[ºÌæÉ}NGg[ñHª`¬³êĨèCPSVTÉÁ¦CS[×®iatrial fibrillation:AfjÍS[e®iatrial flutter:AFjðø«N±µC»ÌêÉSºpiventricular tachycardia:VTjâSº×®iventricular fibrillation:VfjðµÂ\«Ì é¾³QÅ é7,11jBA ÉY·éàÌÍCAFyÑS[piatrial tachycardia: ATjÌS[àÌGg[pª°çêé10jª A É¢ÄÍÊÌ@ïÉ¢ðs¢C±±ÅÍ @ ÌÝðæµ¢½¢B
@±±ÅÍC[ºÌæÌ}NGg[@ÉæèPSVTðN±·aÔðu[ºp¬«¾³iatrioventricular tachyarrhythmias:AVTjvÆÄÑCAVTÉæ讧CßÜ¢C¸_Ìz®ÔÌÙíðu¬ÍwI»Ûihemodynamic phenomena:HDPjvÆÄÔ±ÆÆ·éB
@HDPðFß½êÍCqóãwIÉCdåÌÌ´öÌêÂÆl¦é׫ŠèCKØÈffÉæèCqóãwK«iȺuK«vÆ¢¤jð»fµÈ¯êÎÈçÈ¢BuK«vÆÍC@ qóƱðÀ{·é½ßÉKvÈSgÌóÔªêè
É é±ÆC·Èí¿C çäéóµºÅÀSÉòs·é½ßÉKvÈ
ÈãÉSgÌóÔª é±ÆCA ±ÌóÔªLøúÔÛ³êéÆ\z³êé±ÆCðw·13jB
@íªÌ¯Ôqóɨ¢ÄCȺÌêÍqóg̸}j
AÉLÚ³êÄ¢ég̸îÉîësKÅ èCqóƱðs¤±ÆªoÈ¢13jB±±É¨¯éusKvÆÍCK¥Åèßçê½ÈºÉ¦·g̸îð½³È¢êðw·B
@@@êß«áµÍ±«Ìãºpisupraventricular tachycardia:SVTjÍAf/AFÍ»Ìùðª éàÌB
@A@WPWÇóQ̤¿Cì«pðº¤àÌCÍ»ÌùðÌ éàÌB
@B@»Ì¼Sd}ãCdåÈS¾³ðèÅ«éàÌB
@C@²¥ÙíÉεÄNPI¡ÃiJe[eSØÄÜpjðsÁ½àÌB
@qó©qàɨ¢ÄCȺÌêÍsKisijÆÈèC¯ÔqóƽÙÈÁ½ÈºÌæ¤ÈàeÆÈÁÄ¢é12jB
@@@p쎫C©ÂÇóðº¤àÌB
@A@±«Ìì«pCAFÍAfB
@B@WPWÇóQÅì«pðº¤àÌB½¾µC¸bicmóâÒÌK«»èjÅÍCWPWÇóQªÈ¢±ÆB
@C@»Ì¼Sd}ãCdåÈS¾³ðèÅ«éàÌB
@sKƳêÄàCqóƱðó]·éÒÍCv̸§¸ðs¢CKvɶġÃðs¢CÇóªÀèµÄ¢é±ÆªmF³êÄ©çCEF[o[iWaiverjR¸ð\¿·é±ÆªÅ«éBEF[o[R¸ÆÍCsKƳê½ÒÉεÄC»ÌÒÌo±yÑ\Íðl¶µÄCR¸ÌÊC»ÌsKªqóÀS𺩳êȢƻè³êéêÉÀèCg̸îÉK·éÆÝÈ·±ÆªÅ«é§xÅ è13jC±±ÅÍCiÌêðuK«ðL·évCsiÌêðuK«ðvÆ\L·éBÁ¦ÄCg̸îÉK·é©»è¢ïÈáÉεÄàCEF[o[R¸ð\¿µC]¿yÑ»èðó¯é±ÆàÅ«é11jBȨC¯lȧxÍ©qàÉà¶Ý·é12,14jBÂÜèCK«ÉÖµÄÚ×È¢ðs¤êÍC´¥EF[o[R¸ðs¤±ÆÉÈéB
@±±ÅÍCàOÌÕ°ãwIm©yÑqóãwIm©Ìõðs¢CAVTªFßçêéáÌK«]¿yÑ»è@𢵽¢BȨC_¶ÍC´¥ÆµÄAVTÌݪFßçêÄ¢éêðzèµÄ¢éÌÅC¼Ìîb¾³ÌûªaÔÉå«Èe¿ðyÚ·êÍCÊr¢ªKvÅ éB
II.@Õ°ãwIm©
@{¢ÉKvÈm©ÉÖµÄÍCåƵÄCuÕ°SdC¶¸ielectrophysiological study:EPSjÉÖ·éKChCiȺuEPSKChCvÆ¢
¤jv21jCus®¬Ìñò¨¡ÃKChCiȺuñò¨¡ÃKChCvÆ¢¤jv23jyÑuJe[eAu[ViȺuAu[VvÆ¢¤jÌKÆèZÉÖ·éKChCiȺuAu[VKChCvÆ¢¤jv22jÉîÃÆæ¢Æl¦çêéBff@yÑ¡Ã@ÌÚ×ÉÖµÄÍCåƵıêçKChCÉ÷éªC»ÌÅàqóãwIÉdvÈðLÚ·éBȨC±êçÌKChCÌÝÅÍ¢·éÌÉs\ªÆl¦çêéÌÅC»Ì¼ÌñàÁ¦éB
@A.@PESðAVT
@1.@aÔ
@Table 1ÉÍY_¶Å浤¾³ð¦µ½B
@AVNRTÍCæVIÉFßé[ºßñd`±Hifast pathwayÆslow pathwayjÌGg[pð¶¶éàÌð¢¤BSlow pathwayðsCfast pathwayðts·éàÌðslow-fastiÍÊí^jAVNRTÆÄÔB»Ìtðfast-slow AVNRTÆÄÑC»Ì¼Cslow-slow AVNRTà¶ÝµC»êçðñÊí^AVNRTÆÄԱƪ éBSlow-fast AVNRTªSÌÌ80%Èãðèßé16jB
@AVRTÍC[ºÔÉæVIÉFßé`±HÆ[ºßÌñÂÌoH̤¿CêûðS[©çSºÉC¼ûðSº©çS[É»±ª`±µGg[«Ìpð¶¶éàÌð¢¤BAVRTðø«N±·àÌƵÄCWPWÇóQª é21jBAVRTÌHÈaÔƵÄCPJRTÍCº[`±ª[ºß-His-Purkinjeh`±nðC·¢`±ÔðàÂ`±Hi¢íäéslow Kent©jðî·éàÌðw·21jB
@ȨCAVNRTyÑAVRTÅPSVTSÌÌ90%ÈãðèßéƳêé10jB
| Table 1.@Disorder schema in this document. |
| @@ [ºp¬«¾³ |
[ºßGg[p |
Êí^:slow-fast |
| iú»±ÇóQðj |
|
ñÊí^:fast-slow |
|
|
ñÊí^:slow-slow |
|
[ºGg[p |
³í`±H |
|
|
PJRT |
| @@ ú»±ÇóQ |
Wolff-Parkinson-WhiteÇóQ |
°« |
|
|
Ô« |
|
|
öÝ« |
|
Lown-Ganong-LevineÇóQ |
|
|
»Ì¼Ìú»±ÇóQ |
|
| @@PJRT:permanent form of junctional atrioventricular reciprocating tachycardiaD |
 |
|
Fig. 1. Algorithm to differentiate narrow QRS tachycardia
AT:atrial tachycardia, PJRT:permanent form of junctional atrioventricular reciprocating tachycardia,
AVNRT:atrioventricular nodal re-entrant tachycardia, ANRT:atrioventricular re-entrant tachycardia imodified from reference 21 and reformedj. |
@2.@ff
@QRS120 msecÌpiS≧100 bpmjÍNarrow QRS pÆÄÎêCPSVTC´«p¬CAFi2:1`±jÉFßçêCVTÉÍFßçêÈ¢BPSVTÌÅàClong RP piQRSg¼OÉPgª éàÌjÍATCPJRTÍfast-slow AVNRTÉCshort RP piQRSg¼ãÉPgª éàÌjÍåƵÄAVRTÍslow-slow AVNRTÉCPgªs¾ÈêÍslow-fast AVNRTÉFßçêé18jBFig. 1ÉÍCnarrow QRS pÌÓÊÌt[`[gð¦·21jBêûCwide QRSpÍCQRS≧120 msecÌpðwµCÊíCVTÌêÅ éªCrubNÌÏs`±ðº¤PSVTÌêà éBPSVTÅÍÊíC[ºð£CQRS≧140 mseci¶rubN^ÅÍCQRS≧160 msecjC¶²ÎÊiÁÉdC²≦|30°jÍFßçê¸CV1U±ÅO«i½¾µCtaller left rabbit eariRsrLg`ð¦·àÌ:¶ÌRgªå«¢àÌjðjð¦·20jB
 |
|
Fig. 1.@TMT results in 264 volunteers ifeasibility studiesj.
a.@Comparison of first and second TMT measurements.
In order to verify the precision of the thermometer we used, healthy volunteers were asked to measure their TMT twice.@We then compared the two measurements.@There was no significant difference between the first and second TMT measurements. TMT:tympanic membrane temperature.
b.@Variation of TMT with environmental temperature.
We also determined whether environmental temperature influenced the TMT of healthy volunteers.@Environmental temperature did not significantly affect TMT values. |
@dvÆÈéÌÍCAVRTÆATÌÓÊÅ éBAT̽ÍìÌSd}Åff³êé±Æ©çCPSVTɪ޳êéꪽ¢BATÍS[àÉÀǵ½ÙídC»±ª100-240 bpmÅ»êCP-PÔÉdÊüª éàÌðw·BSd}ãCPgÍQRSgÌOɾÄÉFßçêéªCSª½¢êÍCæsSÌTgÆdÈès¾Äȱƪ èCEPSÉæéfast-slow AVNRTÍPJRTÆÌÓʪKvÉÈéêª é32jB
@ȨCPJRTÍCSd}ãCIICIIICaVFCV5-6ÅA«Pgª©çêéincessant typeip^jÌlong RPpÅ é4jB
@B.@PES
@1.@aÔ
@PESÍCWPWÇóQyÑ»Ìn8jC[ºÔÉ[ºßÈOÌ`±HðFßéàÌiSd}ãCPRÔÌZkð¦·àÌjðw·æ¤Å éªCèÜÁ½©ðÉRµ¢B»ÝCWPWÇóQ̼CLGLÇóQɪ޷é©ðª é21jB
@WPWÇóQÍC]Kent©RÉæéàÌÆl¦çêÄ¢½ªCÅßÍC©}Sº`±Hifasciculoventricular pathway:FVPjRÌaÔàÜÜêéÆ·é©ðª é27jB
@Kent©:æVIÉFßçêéS[ÆSºÔÉ[ºßÈOÌ`±HB
@FVP:[ºßÍHis©©çSºØÖéüÛ©ðw·àÌƳêéªCs«¸`±Á«ðL·é`±HSÊðw·Æ¢¤Ó©à é21jB
@¸`±:Oh©çhªüéÜÅÌÔiAújªZÈéÆ`±Ôª·Èé±ÆðwµC[ºßâ´ßCß×EÁLÌ`±Á«ðw·B
@LGLÇóQ̬öÉ¢ÄÍCJamesüÛCS[-His©`±HC[ºßá`¬C[ºß`±´iienhanced atrioventricular nodal conduction:EAVNCjÍ[ºßñd`±H̬`±Hifast pathwayjÌ`±´iª°çêCPRÔÌZkÉ¢Ä̬͡öªl¦çêÄ¢é21jB
@JamesüÛ:´ßÆ[ºßðA·é3{ÌßÔHiOCCãjÌàCãßÔHª´ßÌã©çoÄC[ºßÌåªðoCpXµÄC»Ìºûųíh`±nÆAµ½`±HB
@2.@ff
@WPWÇóQÍCSd}ãCSºú»±ð½f·éC@ short PRÔiPR120 msecjCA QRS100 msecCB f^gCð¦µCÊíCÇóðº¤àÌƳêé21jB½¾µC{¢É¨¢ÄͳÇóÌêàWPWÇóQÆ¢¤±ÆÆ·éB»ÌÁ¥ISd}©ªPíIÉFßçêé°«WPWÇóQCÔIÉo»·éÔ«WPWÇóQC`±HͶݷ骻Ìs«`±ðL³¸ts«`±ÌÝðLµÁ¥ISd}©ðLµÈ¢öÝ«WPWÇóQÆ¢¤ªÞª é21jBȨCRosenbaumçÍ»ÌSd}g`©çȺÌæ¤ÉªÞµÄ¢é26jB
@A^:V1ÅRp^[iR/Sä1jð¦·àÌB
@B^:V1ÅrS p^[iR/Sä1jð¦·àÌB
@PESÉÍCWPWÇóQ̼Cshort PRÔiPR120 msecjðFßéàÌÌQRSgͳíÅ éLGLÇóQÆ¢¤¾³TOª èC»ÌffÉÍPSVTCAf/AFÌùðL·éKvª éƳêé7jB½¾µC{¢É¨¢ÄͳÇóÌêàLGLÇóQÆ¢¤±ÆÆ·éB
@ÂÜèCPSVTðǵĢȢAVTÍCPESÈOff³êÈ¢±ÆÆÈèCPESÈOÌAVTÍPSVTÌÇð«Á©¯Éff³êéàÌÅ éB
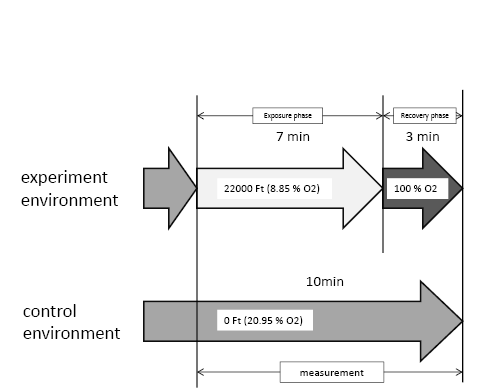
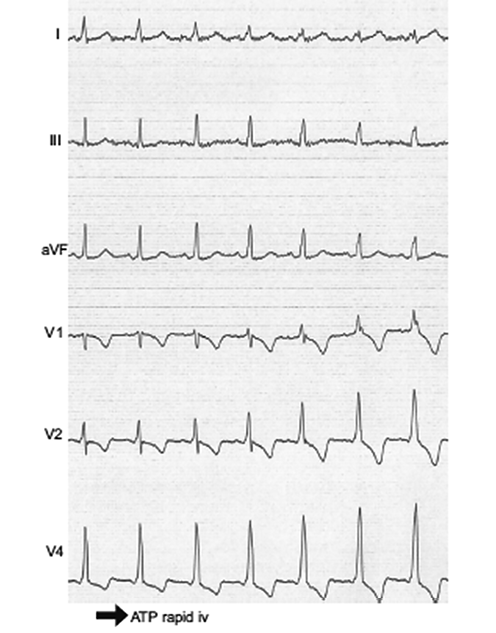
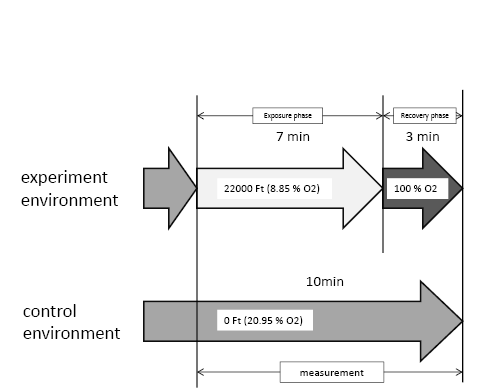
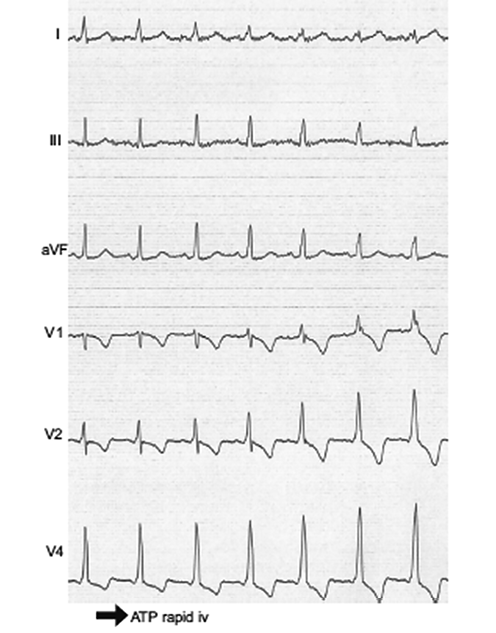
@³ÇóÌPESÌ]¿ÉAfmVeXgÌLp«ð壷é¤Òà¢é6,27jBAfmVeXgÆÍCAfmVO_ð}¬Oa·é±ÆÅêIÉ[ºubNð쬵CQRSgÌ`ÔÌÏ»ªFßçê½êC`±HÉGg[@\ðL·éÆ]¿·éàÌÅ é27jBFig. 2ÉÍCAfmVO_ð}¬OaÉæéQRSgÌ`ÔÌϻ𦵽áð¦·27jB
 |
|
Fig. 2. Alteration of QRS waveform due to adenosine triphosphate iATPj
The QRS interval becomes wider but the PR interval remains unchanged due to atrioventricular block by rapid ATP infusion iadenosine testj, which is diagnosed as having a functional accessory pathwayisj icitation from reference 27j. |
@3.@WPWÇóQÌ\ã
@AfªU³ê½³ÇóÌWPWÇóQ𦵽á̤¿Cñ3NÌoßÏ@É©Rìªo»µ½8á3áÉVfÍËRª¶µ½Æ¢¤ñª è24jC»ÝÍCAf/AFÌùª éêÍSËRÌë¯QÆ¢¤F¯Å éBAf/AFÌùÈOÌë¯QÌîÍ»Ým§³êĢȢªCKent©Ìs«LøsúiúOhÉæÁÄ»±ª¶¶È¢Å·ÌAújª250Í270 msecȺC¡`±HCEbsteinï`¹áÍêÊIÉë¯QƳêéB©Rì é¢ÍUÉæéAfÌÅZRRÔuÉ¢ÄÍ220C240Í250 msecȺðë¯QÌîÆ·éà̪ éBEPSÅCSºÌ¢AfâAVRTªU³êéêâCAfªU³êKent©s«Løsúª300 msecȺÌêàë¯QÅ éÆÌñà é21jB
@WPWÇóQÌÉCPSVTCAf/AFðø«N±·ë¯ÍȢƳêéFVPÉæéà̪ÜÜêÄ¢é±ÆªwE³êÄ¢éBSuzukiçÍC³Çó©ÂQRS≦120 msecÌWPWÇóQ30¼i½ÏNî12.7ÎjÉAfmVeXgðs¢CWPWÇóQi`±HÉ@\ðL·éjÆFVPi`±HÉ@\ðLµÈ¢jÌÓÊðsÁ½Æ±ëC7ái23.3%jªWPWÇóQC23ái76.7%jªFVPÅ Á½BRosenbaum A^𦵽áÍ6áSõi100%jªWPWÇóQCB^𦵽áÍ24á23áªi96%jªFVPÅ Á½BB^𦵽1áÌWPWÇóQÍCAfmVeXgžç©ÉWPWÇóQƪ©éå«Èf^gÆQRS120 msecð¦µÄ¢½B±ÌÊæèCQRS≦120 msecÌB^ÍTËFVPÅ ë¤Æq×Ä¢é27jB
@Á¦ÄȺÌæ¤Él@³êÄ¢éB
@@@gbh~^®×Sd}ÍC[º`±ª°Ý»·é±Æ©çCf^gª¬³ÈèCQRSª·ÈéÆ\z³êéªCLpÅÍÈ©Á½B
@A@z^[Sd}ðÀ{µCS[úOûk̶âSÌϻɶQRSgÌ`ÔÌÏ»ªFßçê½êÍWPWÇóQÆffÅ«éB©ÂCSªÈÈÁ½ÍCWPWÇóQÅÍCf^gª¾ÉÈé͸ŠéB
@CohençÉæéìÆïÍCWPWÇóQ𦵽8Ωç21ÎÜÅÌáNÒÉηéæµ¢iSËRÌ\hjÉ¢ĩðð¦µCȺÌÊèÆÈÁÄ¢é25jB
@@@³ÇóÌÔ«WPWÇóQÌêÍoßÏ@B
@A@³ÇóÌ°«WPWÇóQÌêÍ^®×¸ðs¢CPESÌتÈÈêÎoßÏ@B»êÈOÍEPSðÀ{B
@B@EPSÉæèCSVTªU³êêÎAu[VÌKª éB
@C@AfÌSd}ãÌÅZRRÔª250 msecȺÌêÍCSËRÌÂ\«ª¢ÌÅAu[VÌKª èC250 msecæè·CEPSÉæèSVTªU³êÈ¢êÍoßÏ@Å梪CSVTðN±·ÆDܵȢÁ¥ª éÒi±±ÅͼÌS¾³ð¹µÄ¢éÒðzèµÄ¢éjÍAu[VðsÁ½ûªÇ¢B
@Á¦ÄßÌñ̪Íðs¢CȺÌæ¤Éq×Ä¢éB
@@@ÁîÆÆàÉ`±HÌ@\ªáº·éÆl¦çêéB
@A@³Çó̬lÌSËRÌNÔǦÍ0%`0.45%Å Á½B
@B@^®×¸Éæéf^gÌÁ¸ÍCKent©Ì·¢s«LøsúÉÖAµÄ¢éB½¾µC^®×ÉæÁÄf^gªÁ¸·éÌÍåƵĬŠéB
@FitzsimmonsçÍCWPWÇóQ𦵽Rpqó]Ò228¼i½ÏNî34.3ÎjÉε½Ï22NÔÇÕ²¸ðsÁ½B»Ì¤¿1¼¾¯ªËRðN±µ½iNÔS¦0.02%jBusymptomsÍSVTi±±ÅÍ3AÈãðw·jvÌùáÌÇÕ²¸ÌSVTÌÇÍ46.3%iNÔǦ2.0%jC³ÇóáÌSVTÌVKÇÍ15.3%iNÔǦ0.7%jÅ Á½BSVTÌVKÇðFß½³Çóá28¼Ì¤¿19¼ÉHDPi67.8%jªFßçê½3jB
@GoudevenosçÍCk¼MVÅWPWÇóQ𦵽157¼i½ÏNî42.5ÎjÉεĽÏ55i4.6NjÏ@ðsÁ½B»±ÉÍ80¼Ìsymptoms ibrief palpitationsjªùðÍoßÏ@ÉFßçê½áÆC77¼ÌoßÏ@ÉsymptomsÍFßçêÈ©Á½áªo^³êÄ¢éB½¾CsymptomsªFßçêÈ¢80¼Ì¤¿CSd}ffãÉßÄsymptomsªFßçê½áÍí¸©3¼µ©¢È©Á½5jBÂÜèCsymptomsªFßçêĢȩÁ½ÌÍC77+3=80¼Å Á½B½Ï4.6NÌoßÏ@Å3¼ªÇµ½±Æ©çC³ÇóáÌsymptomsÌNÔǦÍ0.8%öxÆÈéBȨCsymptomsÌNîÍTË40΢ŠÁ½ÆñµÄ¢é5jB
@MungerçÍC³ÇóÌWPWÇóQ53¼i½ÏNî33ÎjÉ537 patient-yearsÏ@ðsÁ½Æ±ëCËRÍFßçê¸C11¼iNÔǦ2.0%jÉsymptomsªFßçê½B»ÌsymptomsÌàóÍC6¼ÉtachycardiaC5¼Élimited palpitationÅ Á½BȨCsymptomsªFßçê½á̽ÏNîÍ25ÎÅ èC40ÎÈãÅÍǪFßçêÈ©Á½ÆñµÄ¢é17jB
@4.@LGLÇóQÌ\ã
@LGLÇóQÅÍCshort PRÔð120 msecȺƵ½êCêÊlÌ2`4%ª±êð½·±Æàñ³êCPRÔÍ©¥_oâò¨Ìe¿àó¯é±ÆC é¢ÍSd}ðÊíÌL^¬xi25 msecjÅL^·éÆPgÌdʪáȾç©Å é±Æ©çC20 msecöx̪èë·ª¶¶¾é±ÆàwE³êÄ¢é9jB
@NielsençÍCCopenhagen General Practitionerfs LaboratoryÅQÆÅ«½11,087¼Ì15ÎÈãÅCAfÌùÌÈ¢ÎÛÒi½ÏNî57ÎC¼ÌS¾³ÌùàÜÞjÉεC½Ï5.7NÔÌÇÕ²¸ðsÁ½B»ÌÊCPRÔªZkÍ·³êêγêéÙÇCjÆàJÈüð`æ¤ÉAfÌǦªÜé±Æ𦵽B»µÄC«Ì121 msecȺQi5% percentileȺjÍClQi148-157 msecjÉä×LÓi믦1.21jÉAfÌÇͽ©Á½ªCj«Ì129 msecȺQi5% percentileȺjÍClQi154-165 msecjÉä×½¢Xü𦵽ªCLÓÅÈ©Á½i믦1.09jBAfðǵ½«Ì121 msecȺQÉCf^gðFß½ÌÍ164¼1¼i0.6%jÅ Á½BNÔǦÍC«Ì121 msecȺQi½ÏNî43Îj0.43%C«Ì122-135 msecQi½ÏNî47Îj0.39%Cj«Ì129 msecȺQi½ÏNî44Îj0.44%Cj«Ì166-179 msecQi³íÍÍC½ÏNî55Îj0.71%Å Á½BÅZÌPRÔÍjÆà104 msecÅ Á½19jB
@GrossmançÍCPESª^íêé59¼if^gª^íêéá15¼Cf^gªÈ¢á44¼C½ÏPRÔ110 msecjÌCXGóRÌcmóâ¶ÉAfmVeXgðÀ{µC·×ÄÌóâ¶É¾ç©È`±HðFß驪Fßçê¸C½Ï35.4Ï@ðsÁ½ªÙíÍFßÈ©Á½ÆñµÄ¢é6jB
@C.@AVTÌ¡Ã
@{¢Å浤¾³iTable 1jÌ¡ÃÍ´¥Au[VÅ éBAu[VÉÖ·éÚ×ÍCAu[VKChCyÑñò¨Ã@KChCÉLÚ³êĨèCAVT̪¡ªúÒÅ«é¡Ã@Å é21,23jBTable 2ÉÍC±êçKChCɨ¯éAu[V̧xðÜÆß½BEPSiAu[VãÌøÊ»èðÜÞjÉÖ·éÚ×ÍCEPSKChCÉLÚ³êÄ¢é21jBȨC±êçÌèZð±±ÅÍuJe[euvÆ¢¤±ÆÆ·éB
@AVNRTyÑWPWÇóQiAVRTjÌAu[VÌèZÍÙÚm§³ê½Æ³êé31jBLGLÇóQÍC»ÌffÉÍPSVTCAf/AFÌùðL·éKvª é±Æ©çCÇóðL·éêÍJe[euÌKÆl¦çêéªCshort PRÔÌÝűêçÌùðLµÈ¢áÉÍCêÊIÉK³êȢƳêÄ¢é30jBµ©µCshort PRÔáÅAf¹ÉVfǪñ³êÄ¢é±ÆÍÓðv·é21jB
| Table 2.@Advisability of catheter ablation in case of atrioventricular tachyarrhythmias. |
|
[ºßGg[p |
WPWÇóQ |
|
| NXI |
1.@¸_ÈÇÌdÄÈÇóâyÇóÅàQOL̵¢áºðº¤pìÌùª éê |
1.@¶½Éë¯ðyڷ믫ª éCܽ͸_ÈÇÌdÄÈÇóðº¤p¬«S[×®â¼ÌS[«p¬«s®¬ª éê |
| 2.@pìª èCò¨¡ÃÌL³ÉÖí縳ҪJe[eAu[Vðó]·éê |
2.@`±Hðîµ½pìª èCZÔÅ©Râ~µÈ¢CÇóðº¤Cpxª½¢CÈÇÌê |
|
3.@`±Hðîµ½pìÍÈ¢ªCnCXNQÅCö¤ðÊ@ÖÌ^]èÈÇCƱàeª³ÒÈOÌl½ÉÖíéÂ\«ª éê |
| NXIIa |
1.@pìÌSd}ªmF³êÄ¢é³ÒÅCdC¶¸ÅpªU³ê¸ñd[ºß`±HÌݪFßçê½ê |
1.@`±Hðîµ½pìÍÈCnCXNQÅàÈ¢ªCS[×®ÇÌÂ\«ÈÇðl¶µÄ³ÒªJe[eAu[Vðó]·éê |
| 2.@¼ÌpÉηédC¶¸Ü½ÍJe[eAu[V¡ÃÉôRU³ê½[ºßGgp |
2.@pìðFßÄàÇóªy÷ÅCZÔÅ©Râ~µCpxàÜêÈê |
| NXI:LvÅ éÆ¢¤ªª èCKÅ é±ÆªêÊɯӳêÄ¢éBNXIIa:LvÅ éÆ¢¤Ó©ª½¢àÌBiJe[eAu[VÌKÆèZÉÖ·éKChCyÑs®¬Ìñò¨¡ÃKChCi2011NüùÅjæèøpj |
III.@qóãwIm©
@qóãwIm©ÅLpÈàÌÍCêÊIÉͯÔqóãw}j
AiManual of Civil Aviation Medicine: ¯ÔqóÌãw]¿ÉÖ·éWIÈ}j
ACåƵĢBÌqóÇ̤Ҫì¬jCqóg̸ãKChiGuide for Aviation Medical Examiners:Äɨ¯éqóg̸}j
AjCÄóREF[o[KChiAir Force Waiver Guide:ÄóRɨ¯éEF[o[R¸\¿Ì½ßÌ}j
AjCÄCREF[o[KChiU. S. Navy Aeromedical Reference and Waiver Guide:ÄCRɨ¯éqóg̸Ìû@yÑEF[o[R¸\¿Ì½ßÌ}j
AjÌ}j
ACRaymanfs Clinical Aviation Medicine̳ÈC_¶Å éB±êçðõµ½ÊC]¿yÑ»è@ì¬ÉLøÈLqÌÝðȺÉq×éB
@ȨCàÌK¥à¢ÉKvÅ é½ßC±±Åq×éB
@A.@¯Ôqóãw}j
A15j
@AVNRTÍCìÍê¶Uɨ¢ÄÄ·éXüª èCmÀÉ®SÉ}§·é±ÆªÅ«È¢½ßCÊíCK«ðBáOƵÄCx`±HÌCüðó¯ÄCEPSÅU³êȯêÎCK«ðL·éÆÅ«éi1.5.23ÌjB
@ßÄWPWÇóQ𦵽êCK«ðƷ׫ŠéBs®¬ÌùªÈC¸¸ÉÙíªÈ¯êÎC¡À@i2¼ÈãÌcmªcÂ\Èqó@jÌƱððtµÄK«ðl¶·é±ÆªÅ«éi1.5.27ÌjB
@³§ÀÌK«ÉÖµÄÍCEPSÅU±«SVTðFßÈ¢±ÆCyÑ`±HLøsúª300 msecæèå«¢±ÆÌؾªKvÅ éBGg[«s®¬Ìùðª éêC`±HÌAu[VÉæèiªÂ\Å éi1.5.28ÌjB
@B.@ÄóREF[o[KCh1j
@Çóª éàÌÍK«ðB3AÈãÌãºúOûkÍÚ×È]¿ðs¤±ÆÆÈÁÄ¢éiSupraventricular TachycardiaÌÍjB
@AVNRTÍCcmóâ¶Åà»ðcmÅàCEF[o[R¸Â\Å éiCatheter Ablation of Tachyarrhythmias and/or Pre-Excitation iWPWjÌÍjB
@WPWÇóQi³ÇóàÜÞjÍsKÅ éBcmóâ¶ÅÍEF[o[R¸Â\Å éªCEPSÌÀ{ªKvÆÈéBȨC»ðcmÉÖµÄÍCEPSÉֵľy³êĢȢiWolff-Parkinson-White iWPWj and Other Pre-Excitation SyndromesÌÍjB
@SVTÉÖµCAu[V¡ÃªsíêĢȢÀèCÇóðº¤àÌÍ´¥IÉK«ðBĵ½±«SVTi±±ÅÍ10ªÈã±SVTðw·jÍK«ðBRg[·é½ßÉRs®¬òªKvÈàÌÍK«ðiSupraventricular TachycardiaÌÍjB
@C.@ÄCREF[o[KCh29j
@ÇóÌ éWPWÇóQÍK«ðB³ÇóÌWPWSd}g`ª êÎCEPSðÜÞ]¿ªKvÅCÙíªÈ¯êÎCEF[o[R¸Â\Å éBEPSÅs®¬ªU³ê½êÍCAu[Vðs¢C¯¶û@ÅU³êÈ¢±Æð¦·Kvª éBService Group 3i¡À@ÀècmjÅ êÎC6ÔÌoßÏ@ÌãÉEF[o[R¸\¿Â\ÆÈéBService Group 1iƱðªÀè³êÈ¢cmjÅ êÎC6ÔÌoßÏ@ãCÄðN±³È¢±Æðؾ·éÞðtµÄEF[o[R¸\¿Â\Å éBÇóðº¤WPWÇóQâLGLÇóQÅEF[o[R¸ðó¯éÉÍCAu[VªKvÅ éB
@f^gðºíÈ¢very short PRÔ iPR100 msecjÍñNPIS]¿ÅÙíªÈ¯êÎKÅ éªCÙíª êÎsKÅCEPSÍAu[VªKvÆÈéB
@s®¬âÇóðºíÈ¢short PRÔ i≧100 msecj ÍK«ðL·éBÈãC]¿ÍsvÅ éi3.19 Pre-excitation SyndromesÌÍjB
@D.@íªÌyðÊÈqóÇiȺuqóÇvÆ¢¤jÌK¥2j
@ÊBu²¥ÙíÌ浢ɢÄvÅÍCÀÃSd}ÅCSºN¹Å êãºN¹Å ê2ÈãÌúOûkª Á½êÉÍz^[Sd}ðs¤±ÆÆÈÁĨèC
@@@5,000/úÈãÌãºúOûkB
@A@SVTi10AÈã©ÂS170/bpmÈãCܽÍ30bÈã±·éàÌj
@ÌÇ¿ç©FßçêêÎsKÅ éB
@EF[o[R¸ÉñoÂ\ÈoßÏ@úÔÍȺÌÊèÅ éB
@@@WPWÇóQÉηéJe[eAu[Vã:6
@A@WPWÇóQÉæépìù:pìÌo»ÌÈ¢óÔÅ6
@E.@qóÇÌKèÉîâ½FitzsimmonsçÌñÌðÍ
@SVTÆÍ10AÈãð¦·àÌðw·æ¤Å éª28jC¾mÈè`ª³êĢȢBäXÍCqóÇÌKè2jðQlÉCHDPð·Æl¦çêéuqóÇîvðȺ̢¸ê©ð½·±ÆÆè`µ½B
@@@㺫Ìs®¬ª10AÈã©ÂS170 bpmÈã𦵽àÌB
@A@㺫Ìs®¬ª30bÈã±µ½àÌiAf/AF/ATðjB
@Fitzsimmonsçñ3j̳Çóáɨ¯éVKÇá̤¿SVTi3AÈãjªL^³ê½18áððÍ·éÆCqóÇîð½·àÌÍ15ái83.3%jÅ Á½B³ÇóáÌSVTÌVKÇÍ15.3%iNÔǦ0.7%jÆñ³êÄ¢éÌÅCqóÇîð½·àÌÍNÔ0.6%öxÆ\z³êéBȨC³Çóáɨ¢ÄCoßÏ@ÉWPWÇóQªÁ¦½áiÔ«WPWÇóQjÍC»¤ÅÈ¢áÉä×ÄCLÓ·ªÈ©Á½ªCSVTÌǪȩÁ½i8.7%Î23%jB³ÇóÌÔ«WPWÇóQÌáððÍ·éÆCSVTi3AÈãjÌVKÇÍNÔ0.2%öxCqóÇîð½·àÌàNÔ0.2%öxÆ\z³êéB
@F.@1%[
@»Ýu1%[vÉîâ½m¦_IÈK«»èðs¤±ÆªCqóãwãÌXN]¿Ìî{IÈl¦ûÆÈÁÄ¢éB¡À@ÌƱÌcmª@\r¸ðN±µ½êðzèµCȺ̢©ç»Ìlͱ«o³ê½B
@ßÌÌÌ¢©çvIÈÌÍ107ÔÉ1ñÌÅN±éƳêÄ¢éB»Ìà1/10ªlIvöÅC³çÉ»Ì1/10ªòsÌ@\r¸ÉæéBÂÜè109ÔÉ1ñÈãÌpxÌ@\r¸ðN±µÄÍÈçȢƳêéBòsÔ̤¿ÁÉë¯ÈúÔÍC£¤Æ
¤ÌÔÅC»êçÍSòsÔÌ10%ÌÝÅ éB±Ìë¯ÈÔɨ¢ÄcÌcmÉ@\r¸ªN±Á½ÆµÄàCßÌ¢©ç¼Ìcmª100ñ̤¿99ñÜÅÍÀSÉcððãÅ«éƳêéBæÁÄC1/1,000C·Èí¿¡À@ÌƱÌêC106ÔÉ1ñÈãÌpxÌÌÍN±·×«ÅÍÈ¢±ÆÆÈéB1NÔÍ8,760ÔÅ éªC10,000i104jÔƵÄl¦éÆCNÔÌ@\r¸Ìm¦ªTË1%ȺŠêÎC@\r¸ÉæéÌðm¦_ãeÅ«é±ÆÉÈé15jB
@±êͯÔqóɨ¯é¡À@ÌƱž¦é±ÆÅ éÌÅCPÀ@íâ©qàÌG@íÉÍÄÍÜçÈ¢B½¾µC©qàÅàA@Ì¡À@ÌƱÉ¢ÄÍCî{IÉ1%[ÉîâÄXN]¿·é±ÆªKÆl¦éB
@ȨC³§ÀitÑðȵjÌK«ðFßéêÍCíÒƯÌ@\r¸Ìm¦Æl¦çêéÅ ë¤B
IV.@m©Éîâ½K«Ìl¦û
@A.@qóÇîÉîâ½K«Ìl¦û
@FitzsimmonsçÌñ3jÅCuSVTi±±ÅÍ3AÈãðw·jvªÏ@³ê½à̤¿C67.8%ÉHDPªFßçêC83.3%ÉqóÇîð½µ½±Æ©çCHDPðFßéóÔÆ¢¤àÌÍCqóÇîÍ»êæè«¢aÔÌSVTª¶Ý·éóµÅ éÆl¦çêéB
@AVTÉæéu®SÈv@\r¸ªN±è¤éÌÍCVT/VFðäN·éæ¤ÈaÔª éêÅ èC±êçÌNÔǦª1%ð´¦éêÍK«ðBÁ¦ÄCHDPðFßéóÔÍCÀSÈqóƱðs¤±ÆÍÅ«È¢±Æ©çC¯lÉHDPÌNÔǦª1%ð´¦éêÍK«ðÆ·é̪KÆl¦çêéB
@®§CßÜ¢C¸_Ì©oÇóª êÎHDPª éÆ¢¦éªCcƱªs¦ÈÈéÂ\«©ç\¿ÒªKØÉ\µÈ¢êà è¾éB»±ÅCHDPÌ©È\ÉÁ¦Cz^[Sd}ÌqÏIȸʩçHDPÌL³ðè·éKvà éBñíÉ¢ïÈ_ÍCÇÌöxÌSVTðuHDPª évÆè`·é©Å éªCãLµ½æ¤ÉCqóÇîªHDPðFßéúÌóÔÆl¦Äæ¢Å ë¤BȨCWPW ÇóQyÑLGL ÇóQÍAfÌë¯öqÅ é±Æ©çCAf̯lÌaÔÅ éAF/ATàÁ¦ÄHDPƷ׫ŠéB
@ÈãÌ¢©çCȺ̢¸ê©ÌêÍuHDPvÆ»fµÄæ¢Å ë¤B
@@@´¾³ÉîÃHDPª éêB
@A@WPW ÇóQÍLGL ÇóQɨ¢ÄAf/AF/ATÌùª éêB
@B@ãLªs¾ÈêÍCoßÏ@i»ÌúÔÌ¢ÍȺÅs¤jÉqóÇîðFß½êB
@qóÇyÑqó©qàÌKèÉLÚ³êÄ¢éu±«Ìãºp/pì/ì«pvÍñíÉBÈ\»Å éªCãLÚð½·àÌÆ·êÎæ¢Å ë¤B
@B.@ñ]¿
@ßÄAVTÌ]¿ðs¤êCîb¾³ÌÚ×È]¿ðs¤Kvª éBÊíuXN[jO¸iSGR[¸Cz^[Sd}Cgbh~^®×Sd}¸jvðÀ{µCîb¾³ª^íê½êÉÍí¿IS]¿ijãw¸C¥®¬¢eCSMRIjðÀ{·é±ÆÆÈéBÈãÌ]¿ÉÄCÕ°ãLÓÈí¿IS¾³ÌÙíªFßçêÈ¢êÍuîb¾³ªFßçêÈ¢vÆ¢¤±ÆÉÈéBîb¾³ªFßçê½êÍC»Ì¡Ãðs¤×«Å éB
@îb¾³Ì¡ÃCJe[euCò¨¡ÃÍoßÏ@ÉÄCÇóªÀèµ½êÍCoßÏ@úÔðݯCz^[Sd}ÅĪȢ±ÆÌmFðs¤BÈãÌêA̬êðC±±ÅÍuñ]¿vÆ¢¤±ÆÆ·éB
@C.@¡Ã
@AVTÌ}NGg[ÌaÔ©çCÁÉcmÉεÄÍAu[Vɨ¯éª¡ÌÂ\«ðl¶·×«Å éB
@qóÇÌEF[o[R¸É¨¢ÄCWPWÇóQÅAu[VðsÁ½êÍC6ÌoßÏ@ÌKèðݯĢé2jB»ÝÌƱëC±ÌúÔÉÄs襁¶Ä¢È¢½ßÃÆl¦çêéªCoßÏ@ð6Ƶ½¾mȪªÈ¢½ßC¡ã¾mȪª êλêÉ]ÁÄÏX·×«Æl¦éB
@D.@K«Ì¢
@AVTÌñ]¿yÑ¡ÃðsÁ½êCÈºÌ @`A ªl¦çêéB
@@@·×ÄÌGg[ñHªEPSÉæÁij@\Æè³êCoßÏ@ÉÄðFßÈ¢êB
@A@@ð½³È¢êB
@1.@HDPÌùª éAVT
@Ī\z³êéÌÅ @ ð½µ½êÍC³§ÀÌK«ðL·éB½¾µCAf/AF/ATÌùª éêCÄÌ°ê©çC´¥ÆµÄ¡À@©ÂáG@íÀèÆ·é׫Šë¤B
@2.@HDPÌùªÈ¢WPWÇóQ
@Je[euª{s³ê½êÍC@ ð½µ½êͳ§ÀÌK«ðL·éBA ÌêÉ¢ÄȺŢ·éB
@±êÜÅÌm©æèCȺÌÊèÆl¦çêéB
@1j@QRS≦120 msecÌB^ÍTËFVPÅ é27jB
@2j@z^[Sd}ÍAfmVeXgÅQRSgÉ`ÔÏ»ªFßçê½êÍ`±HÉ@\ª éÆl¦çêé27jB
@3j@¬lɨ¢ÄPSVTÌùªÈ¢WPWÇóQÌSËRÍCÙÆñÇN±çÈ¢3,5,17,25jB
@4j@CohençÌìÆïÌ©ðÍSËRÉåáðu¢Ä¨èC^®×¸ÅÙíªFßçêÈ©Á½ÆµÄàCHDPðÛè·éÉÍçÈ¢B½¾µC^®×Sd}¸ðÀ{µÄCf^gªÁ¸·éÌÅ êÎC`±HÌ@\ªá¢Æl¦çêéB©ÂCÁîÆÆàÉ`±HÌ@\ªáº·éÆl¦çêé25jB
@5j@Goudevenosç24jyÑMungerçÌñ17j©çCusymptomsÍSVTvÌùªÈ¢40ÎÈãÍusymptomsÍSVTvªÙÚN±çÈ¢Æl¦çêéªC40΢ŠêÎêèÌm¦iNÔ0.7`2%öxjÅdÇxªs¾ÌusymptomsÍSVTvÍN±è¤é3,5,17jB½¾µCy÷ÈáâWPWÇóQɺíÈ¢àÌàÜÜêéÆl¦çêCäXªè`µ½HDPÍC»êæèàÈ¢Æl¦çêéBȨCÅàcmɦµ½FitzsimmonsçÌñ3jÌäXÉæéðÍÅÍC³ÇóáÌHDPÌVKǦÍNÔ0.6%öxÅ Á½B³ÇóáÌÔ«WPWÇóQɨ¯éäXªè`µ½HDPÌVKǦÍNÔ0.2%öxÅ Á½B
@ãLÌ©ð©çCêÊZ¯Ì40ÎÈãÍÙÚHDPðǵȢ±Æ©çCK«ðL·éªCGrfXÌÈ¢G@íðƵ½ûªæ¢Å ë¤BêûCVKǵⷢÌÍ40΢ÌáNÒwÅ èCco±Ìó¢á¢cÒÉHDPªN±Á½êÉÍCÌÉÂȪèâ·¢Æl¦çêéB½¾µCusymptomsÍSVTvÌNÔǦª1%ÈãÌÂ\«àÛèÅ«È¢ªCÀÛÌHDPð¦·àÌÌǦÍCFitzsimmonsçÌñ3jÉæêÎ1%¢Æl¦çêéBÔ«WPWÇóQÌêÍCHDPÌpxͳçÉá¢Æl¦çêéB]ÁÄC40΢ÌêÍC´¥ÆµÄ¡À@©ÂáG@íÀèÌK«ðL·éB½¾µCȺÌêɳ§ÀÌK«ðL·éƵÄàæ¢Å ë¤B
@1j@QRS≦120 msec©ÂRosenbaum B^B
@2j@z^[Sd}ÍAfmVeXgðÀ{µCQRSg`Ì`ÔÌÏ»ðF߸C©}Sº`±Hªè³êéêB
@3j@Ô«WPWÇóQÍ^®×¸Éæèf^gÌÁ¸C`±HÌ·¢s«Løsúªè³êéêB
@3.@HDPÌùªÈ¢LGLÇóQ
@Je[euª{s³ê½êÍC@ ð½µ½êͳ§ÀÌK«ðL·éBA ÌêÉ¢ÄȺŢ·éB
@NielsençÌñ19jÍCf^g𦵽áÍ0.6%µ©ÈCÀãLGLÇóQ̢ƯÆl¦çêéB±±ÅÍCshort PRÔªZÈêÎÈéÙÇCáNÒijÆà40ãjÌAfÌǦª¢BNielsençÌñððÍ·éÆCAfÌNÔǦÍC1%¢Å èC«Ìshort PRÔQi≦121 msecjƳíQi122-135 msecjªÙگŠèCj«Ìshort PRÔQi≦129 msecjͳíQi166-179 msecjÆä×ÄCáNŠ骾¯NÔǦªá¢BÈã̱ƩçÉ[ÉPRÔªZ¢Qð¯ÎCT˳íQƯÌAfÌǦÆl¦çêéB
@ÄCREF[o[KChÅÍCvery short PRÔ iPR100 msecjÌêÍñNPIS]¿ªKvÅ èCshort PRÔ i≧100 msecjÌêͳ§ÀÌK«ðL·éƵĢéB±êÍNielsençÌñðl¶·éƱÌæ¤ÈàeÆÈèCíªÅà±êÉ·êÎæ¢Å ë¤B½¾CPRÔ̪èÍë·ª è9jCNielsençÌñ19jÌÅÌPRÔÍ104 msecÅ Á½±Æ©çC110 msecöxð«EƵC±ê¢ðqóãwIÈLGLÇóQÆ·é׫Šë¤B½¾µCSd}ÉÍ20 msecöx̪èë·ª¶¶¾é±Æ©ç9jBJèÔµ¸ðsÁÄff·é׫ŠéB
@LGLÇóQÆff³ê½êÅàCNielsençÌñ19j©çAfÌǦªí¸©Éãªé¾¯Å é±Æ©çC¡À@©ÂáG@íÀèÌK«ðL·éBGrossmançÌñ6j©çCAfmVeXgÍ`±HÌL³ÌèÉLpÅ éÆl¦çêé±Æ©çCz^[Sd}ÍAfmVeXgÌÊ©çCQRSg`Ì`ÔÌÏ»ðF߸C¾È`±HªÈ¢Æè³êéêͳ§ÀÌK«ðL·éƵÄæ¢Å ë¤B
@F.@AVTÌK«»èÄ
@ÈãÌ¢ð¥Ü¦CAVTÌK«»èÄðTable 3ɦµ½BȨCè`µ½HDPðFßÈ©Á½êÅàCÕ°ãwIÉJe[euªKvƳê½êÍÀ{·×«Å éB
| Table 3.@Proposed procedure of aeromedical fitness for the evaluation and assessment of atrioventricular tachyarrhythmias. |
| I.@[ºp¬«¾³É¨¯é¬ÍwI»ÛiHemodynamic Phenomena:HDPjÌùÌè` |
| @Ⱥ̢¸ê©ð½·àÌðw·B |
|
A.@®§CßÜ¢C¸_Ìz®ÔÌÙíðº¤[ºp¬«¾³Ìùª éê |
|
B.@WPW ÇóQÍLGL ÇóQɨ¢ÄS[×®/S[e®/S[pÌùª éê |
|
C.@ãLªs¾ÈêÍCoßÏ@1jÉÈºÌ @`B ¢¸ê©ðFß½ê |
|
@@@@㺫Ìs®¬ª10AÈã©ÂS170 bpmÈã𦵽àÌ |
|
@@A@㺫Ìs®¬ª30bÈã±µ½àÌiS[×®/S[e®/S[p2jðj |
|
@@B@WPW ÇóQÍLGL ÇóQɨ¢ÄS[×®/S[e®/S[pðFß½ê |
| II.@qóãwɨ¯éffî |
| @A.@WPWÇóQ |
|
@@HDPÌùÌL³Íâí¸CÀÃSd}ãCshort PRÔiPR120 msecjCQRS100 msecyÑf^gð¦·êB |
| @B.@LGLÇóQ |
|
@@HDPÌùÌL³Íâí¸CãLµ½WPWÇóQÌî𽳸CJèÔµÀÃSd}ðªèµ½ÌÉàÖíç¸very short PRÔ iPR110 msecöxjðPíIÉFßéêB |
| @C.@ãLÈOÌ[ºp¬«¾³ |
|
@qóãwK«ðÆ»fµCSdC¶w¸Éæé]¿ðv·éB |
| III.@[ºp¬«¾³ÌqóãwK«»èvÌ |
| @A.@HDPÌùª éê |
|
@@1.@S[×®/S[e®/S[pÌù2j |
|
@@@@Je[eAu[VÌÀ{ÌL³ðâí¸C·×ÄÌGg[ñHªSdC¶w¸ÉæÁij@\Æè³êCoßÏ@1jÉHDPðFßÈ¢êC¡À@©ÂáG@í3jÀèÌqóãwK«ðL·éB |
|
@@2.@ãLÈO |
|
@@@@Je[eAu[VðÀ{µC·×ÄÌGg[ñHªSdC¶w¸ÉæÁij@\Æè³êCoßÏ@1jÉHDPðFßÈ¢êÍC³§ÀÌqóãwK«ðL·éB |
| @B.@HDP흻颐4j |
|
@@1.@SdC¶w¸ðÀ{µÄ¢È¢WPWÇóQ |
|
@@@@40ÎÈã:qóãwK«ðL·é5jB½¾µCÈºÌ @`B ÌêÍC³§ÀÌqóãwK«ðL·éƵÄàæ¢B |
|
@@@@40΢:¡À@©ÂáG@í3jÀèÌqóãwK«ðL·éB½¾µCÈºÌ @`B ÌêÍC³§ÀÌqóãwK«ðL·éƵÄàæ¢B |
|
@@@@QRS≦120 msec©ÂRosenbaum B^B |
|
@@A@z^[Sd}ÍAfmVeXgðÀ{µCQRSg`Ì`ÔÌÏ»ðF߸C©}Sº`±Hªè³êéêB |
|
@@B@Ô«WPWÇóQÍ^®×¸Éæèf^gÌÁ¸C`±HÌ·¢s«Løsúªè³êéêB |
|
@@2.@SdC¶w¸ðÀ{µÄ¢È¢LGLÇóQ |
|
@@@@oßÏ@1jðÀ{µCHDPðFßȯêΡÀ@©ÂáG@í3jÀèÌqóãwK«ðL·éB½¾µCz^[Sd}ÍAfmVeXgÌÊ©çCQRSg`Ì`ÔÌÏ»ðF߸C¾È`±HªÈ¢Æè³êéêͳ§ÀÌqóãwK«ðL·éƵÄæ¢B |
|
@@3.@SdC¶w¸ðÀ{µ½WPWÇóQÍLGLÇóQ |
|
@@@@·×ÄÌGg[ñHª³@\Å é±ÆªSdC¶w¸ÉæÁÄè³ê½êͳ§ÀÌqóãwK«ðL·éB |
| tL |
|
EoßÏ@ðKvƵȢêÅàCKvɶÄoßÏ@ðÀ{µ½ûªÀSÆl¦çêéB |
|
EEbsteinï`ÌêÍS@\àÜß½¸¸ðs¤×«Å éB |
| L |
|
@1j@oßÏ@úÔÍ6ªKØÆl¦çêC»ÌúÔÍ1Ìz^[Sd}ðÀ{·é׫ŠéB |
|
@2j@S[×®/S[e®/S[pÌùÍsKÅ éBWPW ÇóQÍLGL ÇóQÈOÌ[ºp¬«¾³Å±êçðFß½êÍCÊr±êçÌ¢ªKvÅ éB |
|
@3j@áG@íÆÍC2.5 GÈãÌG@®ðsíÈ¢@íðw·B |
|
@4j@è`µ½HDPðFßÈ©Á½êÅàCÕ°ãwIÉJe[eAu[VÍSdC¶w¸ªKvƳê½êÍÀ{·×«Å éB |
|
@5j@G@íðÎÛƵ½GrfXªÈ¢½ßCáG@íÉÀèƵ½ûªæ¢Æl¦çêéB |
|
V.@IíèÉ
@¡ñCåƵÄWPWÇóQðÎÛƵ½AVTÌK«]¿yÑ»è@Ì¢ðCàOÌÕ°ãwIm©¨æÑqóãwIm©ÉîâÄsÁ½BK«Ì»è@ÖÍCÂ\ÈÀèÈwIªÉîâ½ê©ððàÁÄCR¸Ì^pðs¤±ÆªdvÅ èC»Ìö³ÈR¸E»èÌÆÈéæ¤ÈñÄðݽB
@íªÅG@íi¯ÔÌÈ|òsÍjÌƱðs¤cmÍCqó©qàÌÝÌ®ÆÈéªCqó©qàÌK¥12jÅÍCcmóâ¶ÌSd}ãWPWÇóQðFß½êÍK«ð±ÆÆÈÁÄ¢éB]ÁÄCqó©qàɨ¢Ä40ÎÈãÅßÄSd}ãWPWÇóQð©³êéáÍÊí è¦È¢±Æ©çCEPSðÀ{µÄ¢È¢WPWÇóQÌ40ÎÈãðáG@íÀèɵÄà^pãÁÉâèªÈ¢Å ë¤B
@íªÌEF[o[R¸ÍCyðÊÈiqóÇjÆhqÈi©qàjɨ¢Ä»ê¼êÌR¸@ÖÅsíêÄ¢éªC»ÌR¸ÍP[XoCP[XÅsíêé±Æª½CÈwIªÉîâ½êIÈKChCÍÈ¢BäXÌñĪC±ÌKChCÌì¬ÉÂȪèCK«]¿E»èÉȺÌøÊð^¦é±ÆðúҵĢéB
@@@K«]¿yÑ»è@̾m»B
@A@»èÌö½«ÌÛB
@B@»èðs¤OÉXN[jOðs¤±ÆÉæèC¸ïpC\¿ÒÌSgIÈSC»èÒÌS̹¸ðh®±ÆªÅ«éB
@{àeÍ2015N6_ÅÌ©ðÉ¢ÄLÚµ½B¡ãÌm©yÑãwÌiàÉÄàeÌÄ¢ðißé׫Æl¦çêéB
VI.@Ó«
@{¢É ½èCzÂíwÉÖ·éMdÈä¾ðèܵ½ôMã¯ÉÞñÅäç\µã°Ü·B
¶@@@£
1j Air Force Waiver Guide, Last Update:28 May 2013.
http://www.wpafb.af.mil/shared/media/document/AFD-130118-045.pdf#search=fAir+Force+Waiver+Guidef, iaccessed 2015-05-28j.
2j ²¥ÙíÌ浢ɢÄCóqæ687C½¬25N1127úD
3j Fitzsimmons, P.J., McWhirter, P.D., Peterson, D.W. and Kruyer, W.B.:The natural history of Wolff-Parkinson-White syndrome in 228 military aviators:a long-term follow-up of 22 years.@Am. Heart J., 142, 530-536, 2001.
4j ¡Ø@¾:[ºGg[«pCÊûzÂíÇóQICú{Õ°Cpp. 578-582, 2007.
5j Goudevenos, J.A., Katsouras, C.S., Graekas, G., Argiri, O., Giogiakas, V. and Sideris, D.A.:Ventricular pre-excitation in the general population:a study on the mode of presentation and clinical course.@Heart, 83, 29-34, 2000.
6j Grossman, A., Wand, O., Matezki, S., Kerner, A., Assa, A. and Glikson, M.:Use of adenosine test for the exclusion of preexcitation syndrome in asymptomatic individuals.@Ann. Noninvasive Electrocardiol., 16, 180-183, 2011.
7j IJ@mC½ö©O:Lown-Ganong-LevineÇóQCÊûzÂíÇóQICú{Õ°Cpp. 212-215, 2007.
8j IJ@mC½ö©O:ú»±ÇóQCÊûzÂíÇóQICú{Õ°Cpp. 413-418, 2007.
9j Josephson, M.E. and Kastor, J.A.:Supraventricular tachycardia in Lown-Ganong-Levine syndrome:atrionodal versus intranodal reentry.@Am. J. Cardiol., 40, 521-527, 1977.
10j غ²îC}Ñ@G:ì«ãº«pCÊûzÂíÇóQICú{Õ°Cpp. 586-589, 2007.
11j Mcª¬Cäã°ê:Wolff-Parkinson-WhiteÇóQCÊûzÂíÇóQICú{Õ°Cpp. 239-243, 2007.
12j qó©qàqóg̸K¥Cqó©qàBæ19Cºa54N83ú iÅIü³:½¬24N329úCqó©qàBæ25jD
13j qóg̸}j
ACóææ531C½¬19N32úiÅIü³:½¬25N1127úCóqæ684jD
14j qóg̸ÉÖ·éPßChq¡Pßæ1Cºa33N16úiÅIü³:½¬26N124úCÈPæ1jD
15j Manual of Civil Aviation Medicine, Third Edition 2012.
http://www.icao.int/safety/aviation-medicine/Documents/8984_cons_en.pdf#search=fManual+of+Civil+Aviation+Medicinef, iaccessed 2015-05-28j.
16j
q÷ê:[ºßGg[pC[ºßGg[pCÊûzÂíÇóQICú{Õ°Cpp. 564-569, 2007.
17j Munger, T.M., Packer, D.L., Hammill, S.C., Feldman, B.J., Bailey, K.R., Ballard, D.J., Holmes, D.R. Jr. and Gersh, B.J.:A population study of the natural history of Wolff-Parkinson-White syndrome in Olmsted County, Minnesota, 1953-1989.@Circulation, 87, 866-873, 1993.
18j pqCFJ_êY:Regular narrow QRS tachycardiaÌÓÊffÆ¡ÃCú{àÈwïGC95, 299-304, 2006.
19j Nielsen, J.B., Pietersen, A., Graff, C., Lind, B., Struijk, J.J., Olesen, M.S., Haunsø, S., Gerds, T.A., Ellinor, P.T., Kober, L., Svendsen, J.H. and Holst, A.G.:Risk of atrial fibrillation as a function of the electrocardiographic PR interval:results from the Copenhagen ECG Study.@Heart Rhythm, 10, 1249-1256, 2013.
20j ¼èõO:Wide QRS pÌÓÊffÆ¡ÃCú{àÈwïGC95, 305-313, 2006.
21j ¬ì@CàV`[CÂÀa²CÆâ`lCÎìVCäã@Cº@ªCÁ¡MYCqjYCFJ_êYCIc²uC¬âäÃvC¬ÑmêC¯cçjC@@OCZF¼ûC½iCö@°C¢SñC½ä^CnÓêYCâ²@ÄCå¼@NCvê\SC¬Ñ`TC¢©a_COì@èCråëbCi£@C¡Ø@¾CÀc³V:Õ°SdC¶¸ÉÖ·éKChCi2011NüùÅjD
http://www.j-circ.or.jp/guideline/pdf/JCS2011_ogawas_h.pdf
iQÆ2015-05-28j.
22j º@ªCàV`[C´¼FCÂÀa²C«d@OCFJ_êYC¯cçjCZF¼ûC´@~Cà¡ lCºDGCìãºFC½ö©OC¼{vCºìTñCRªõêCåac^ºC²XØ^áC¢©a_Cêc@_CråëbCIJ@mCV@CÆâ`lCNct
CäTVCOcºGY:Je[eAu[VÌKÆèZÉÖ·éKChCD
http://www.j-circ.or.jp/guideline/pdf/JCS2012_okumura_h.pdfiQÆ2015-05-28j.
23j º@ªCàV`[CÂÀa²C鶲Cå¼@NCÁ¡MYC´
ºFCVc@²C´½vC¼{vCºìTñCÎìVCâ@@C~º@Cì¤áCIc²uC²XØ^áCuê@C¯cçjCZF¼ûC¢SñCºDGCëìTêC½ö©OCå]@§C}Ñ@GCغ@CÊíYCcÎv:s®¬Ìñò¨¡ÃKChCi2011NüùÅj.
http://www.j-circ.or.jp/guideline/pdf/JCS2011_okumura_d.pdfiQÆ2015-05-28j.
24j Pappone, C., Santinelli, V., Manguso, F., Augello, G., Santinelli, O., Vicedomini, G., Gulletta, S., Mazzone, P., Tortoriello, V., Pappone, A., Dicandia, C. and Rosanio, S.:A randomized study of prophylactic catheter ablation in asymptomatic patients with the Wolff-Parkinson-White syndrome.@N. Engl. J. Med., 349, 1803-1811, 2003.
25j Pediatric and Congenital Electrophysiology Society iPACESj;Heart Rhythm Society iHRSj;American College of Cardiology Foundation iACCFj;American Heart Association iAHAj;American Academy of Pediatrics iAAPj;Canadian Heart Rhythm Society iCHRSj, Cohen, M.I., Triedman, J.K., Cannon, B.C., Davis, A.M., Drago, F., Janousek, J., Klein, G.J., Law, I.H., Morady, F.J., Paul, T., Perry, J.C., Sanatani, S. and Tanel, R.E.:PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White iWPW, ventricular preexcitationj electrocardiographic pattern:developed in partnership between the Pediatric and Congenital Electrophysiology Society iPACESj and the Heart Rhythm Society iHRSj. Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology Foundation iACCFj, the American Heart Association iAHAj, the American Academy of Pediatrics iAAPj, and the Canadian Heart Rhythm Society iCHRSj.@Heart Rhythm, 9, 1006-1024, 2012.
26j Rosenbaum, F.F., Hecht, H.H. and Wilson, F.N.:The potential variations of the thorax and the esophagus in anomalous atrioventricular excitation iWolff-Parkinson-White syndromej.@Am. Heart J., 29, 281-326, 1945.
27j Suzuki, T., Nakamura, Y., Yoshida, S., Yoshida, Y. and Shintaku, H.:Differentiating fasciculoventricular pathway from Wolff-Parkinson-White syndrome by electrocardiography.@Heart Rhythm, 11, 686-690, 2014.
28j cç³WvC¡cj:úOûkmS[«C[ºÚ«CSº«nCÊûzÂíÇóQICú{Õ°Cpp. 299-296.
29j U. S. Navy Aeromedical Reference and Waiver Guide, April 30, 2015.
http://www.med.navy.mil/sites/nmotc/nami/arwg/Documents/Complete_Waiver_Guide_150430.pdf, iaccessed 2015-05-28j.
30j Wiener, I.:Syndromes of Lown-Ganong-Levine and enhanced atrioventricular nodal conduction.@Am. J. Cardiol., 52, 637-639, 1983.
31j RàNÆ:ÀnãÆÉßçêéJe[eAu[V¡ÃÌm¯ÆúífÃÖÌpCAu[VŪ¡ª¾çêâ·¢pƾçêÉ¢pCMedical Practice, 27, 1835-1840, 2010.
32j gêNTC´
ºFC¼èv¿:¶[N¹S[pBÊûzÂíÇóQICú{Õ°Cpp. 338-341, 2007.
Aæ:§359-8513@éʧòsÀØ3-2
@@@hqãÈåwZhqãw¤Z^[Ùí«q¶¤å
@@@îàc@Mv
@@@E-mail:takada@ndmc.ac.jp